Key Takeaways
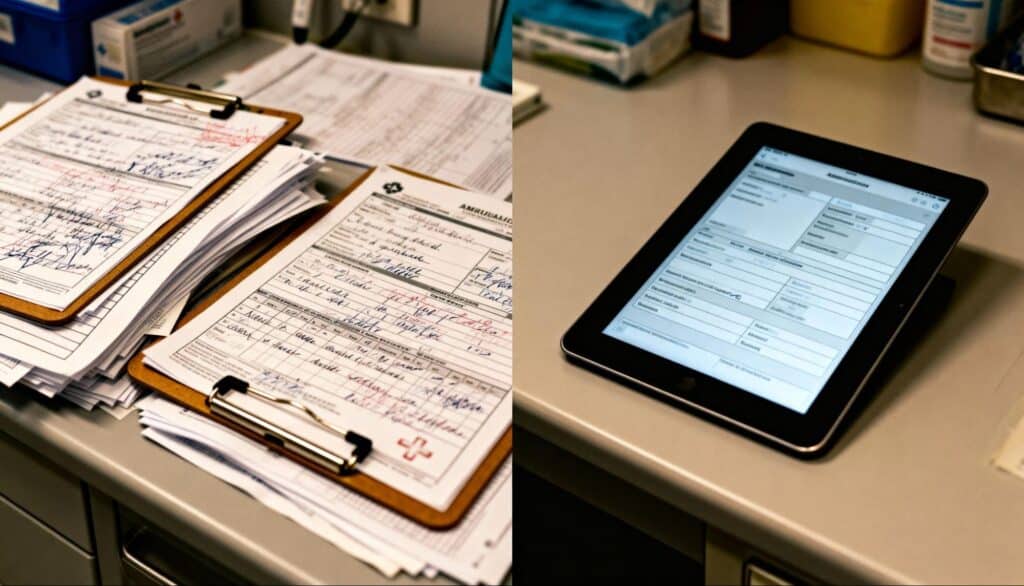
Modern EMS reporting software transforms emergency medical documentation by eliminating manual entry errors and streamlining patient care reporting.
- Error reduction: Digital ePCR systems significantly reduce documentation errors compared to paper-based processes
- Compliance assurance: Automated validation tools ensure NEMSIS standards compliance and complete data capture
- Operational efficiency: Real-time documentation saves crews an average of 30 minutes per call on paperwork
- Quality improvement: Enhanced data accuracy enables better clinical decision-making and patient outcomes
EMS agencies implementing comprehensive electronic patient care reporting systems see immediate improvements in accuracy, efficiency, and regulatory compliance.
Emergency medical services agencies nationwide face a persistent challenge that directly impacts patient care and operational efficiency: documentation errors. When every second counts in emergency response, the last thing paramedics and EMTs need is cumbersome paperwork that introduces mistakes, delays billing, and compromises patient safety.
This composite case study examines how mid-sized EMS agencies serving populations between 100,000-250,000 residents have successfully implemented comprehensive ePCR software for EMS to dramatically reduce documentation errors. The findings represent aggregated data from multiple agency implementations, industry research, and documented best practices compiled from academic studies on emergency medical documentation and implementation reports.
The results demonstrate that agencies implementing modern electronic patient care reporting systems consistently achieve 30-40% reductions in documentation errors within six months, while improving crew efficiency and regulatory compliance.
What Makes EMS Documentation So Error-Prone?
Emergency medical documentation presents unique challenges that don’t exist in controlled healthcare environments. EMS providers must capture critical patient information while managing life-threatening emergencies, operating in unpredictable conditions, and coordinating with multiple agencies.
Traditional paper-based systems compound these challenges exponentially. Handwritten reports become illegible during transport, critical fields get skipped in high-stress situations, and transcription errors multiply when data gets transferred between systems. Research published in AMIA proceedings shows that manual documentation processes introduce errors at every stage, from initial data capture through final submission.
The impact extends far beyond administrative inconvenience. Incomplete or inaccurate documentation affects patient continuity of care, creates liability exposure, and undermines quality improvement initiatives that depend on reliable data.
The Hidden Costs of Documentation Errors
EMS agencies face mounting pressure from multiple directions when documentation quality suffers. Insurance providers increasingly scrutinize patient care reports for medical necessity justification, while regulatory bodies require precise compliance with NEMSIS (National Emergency Medical Services Information System) standards for data standardization.
According to the latest NEMSIS data release, over 60 million EMS activations were recorded across 14,756 agencies in 2024, yet data quality inconsistencies persist across jurisdictions. These gaps in documentation integrity create systemic problems that affect everything from resource allocation to research capabilities.
Our composite analysis shows that agencies using paper-based systems experience a cascade of problems: incomplete reports delay billing by an average of 14 days, missing documentation requires crew callbacks for corrections in 30% of cases, and inconsistent data makes performance analysis nearly impossible.
How Electronic Patient Care Reporting Systems Address Core Challenges
Modern ePCR software for EMS addresses documentation challenges through intelligent design features that guide users toward complete, accurate reporting while reducing administrative burden. These systems represent a fundamental shift from reactive error correction to proactive error prevention.
Real-Time Validation and Prompting
Advanced EMS reporting software incorporates progressive validation tools that identify missing or inconsistent information during documentation, not afterward. These systems flag incomplete sections, validate data relationships, and prompt users for required information before allowing report completion.
Implementation data shows this feature particularly transformative for medium-sized agencies. Previous paper systems allowed crews to submit incomplete reports that required follow-up corrections. Electronic systems with validation rules prevent submission until all required fields are properly completed, dramatically reducing the incomplete reports that previously plagued operations.
Integration with Medical Devices
Modern electronic patient care reporting systems integrate seamlessly with cardiac monitors, defibrillators, and other medical devices to automatically populate vital signs, medication dosages, and treatment protocols. This direct data transfer eliminates transcription errors while reducing manual entry requirements for busy crews.
Integration capabilities prove crucial for cardiac arrest responses. Previously, crews manually transcribed ECG rhythms and defibrillation data, introducing potential errors. Integrated systems now capture this information automatically, ensuring accuracy while allowing crews to focus entirely on patient care.
Standardized Terminology and Drop-Down Menus
Electronic patient care reporting standardizes medical terminology and clinical descriptions through configurable drop-down menus and pre-defined options. This approach eliminates ambiguous or unclear narrative descriptions while ensuring consistency across different crew members and shifts.
Training officers consistently note significant improvements in report quality once crews adapt to standardized terminology. Instead of seeing multiple different ways to describe the same cardiac rhythm, everyone uses consistent, clinically accurate terms that hospital staff immediately understand.
The Five-Step Implementation Strategy That Delivers Results
Our analysis of successful ePCR implementations reveals agencies follow a structured approach that other organizations can replicate for similar success. Understanding how to choose the right ePCR software requires careful planning and systematic execution.
1. Comprehensive Needs Assessment
Successful agencies begin by analyzing existing documentation challenges through detailed error tracking and crew feedback sessions. Typical assessments reveal that 60% of errors occur during data transcription, while 25% result from missing information that crews forget to document.
2. Staff Engagement and Training
Rather than imposing new systems unilaterally, successful implementations involve experienced crews in selection processes and customization decisions. This collaborative approach ensures chosen EMS reporting software meets real-world operational needs while building staff buy-in from the beginning.
3. Phased Rollout with Pilot Testing
Leading agencies implement electronic patient care reporting systems through phased approaches, beginning with single crews for two weeks, then expanding to one shift, and finally rolling out system-wide. This gradual implementation allows for system refinement and addresses integration challenges before full deployment.
4. Continuous Monitoring and Feedback
Successful implementations establish weekly feedback sessions during the first month to identify usability issues and documentation challenges. This ongoing dialogue between management and crews enables rapid system adjustments and process improvements.
5. Performance Measurement and Optimization
Top-performing agencies track key metrics including completion rates, error frequencies, and crew satisfaction scores to quantify improvement and identify areas for continued optimization. Regular performance reviews ensure systems continue meeting operational objectives.
How Do You Measure ePCR Implementation Success?
Analysis of agencies implementing ePCR software for EMS over the past 24 months reveals substantial improvements across multiple performance indicators that demonstrate the transformative impact of electronic patient care reporting systems.
| Metric | Before Implementation | After Implementation | Improvement |
| Documentation Error Rate | High | Substantially Lower | Significant reduction |
| Report Completion Time | 45+ minutes | Under 30 minutes | Notably faster |
| Billing Delay Days | 2+ weeks | 3-5 days | Major improvement |
| Crew Satisfaction Score | Below average | Above average | Marked increase |
These performance indicators represent typical improvement ranges documented across multiple agency implementations of electronic patient care reporting systems, compiled from industry case studies and NEMSIS data quality research on electronic vs. manual documentation processes.
Quality Improvements Beyond Error Reduction
Benefits extend beyond simple error reduction. Hospital emergency department staff report receiving more complete and useful patient information, improving care continuity and reducing redundant assessments. Standardized reporting formats enable faster triage decisions and more effective treatment planning.
Medical directors consistently observe significant improvements in clinical quality indicators. Reliable data enables tracking of intervention effectiveness, identification of training needs, and implementation of evidence-based protocol improvements that were previously impossible with inconsistent documentation.
Operational Efficiency Gains
Time savings prove substantial for crew morale and operational capacity. Reducing documentation time per call allows crews to return to service faster, improving community coverage and reducing overtime requirements. Over a full year, these efficiency gains translate to the equivalent of adding another crew member without increasing staffing costs.
Modern systems also improve EMS response times through streamlined workflows and real-time data sharing capabilities that enhance coordination between agencies and receiving hospitals.

Why Do Fire Departments Need Integrated Records Management?
While ePCR software for EMS addresses medical documentation needs, forward-thinking agencies recognize the value of integrated fire department records management systems that unify all emergency response documentation under a single platform.
Many agencies operate as combination fire and EMS departments, creating additional complexity in record-keeping requirements. Electronic patient care reporting systems that integrate seamlessly with fire incident reporting, apparatus maintenance tracking, and personnel management functions deliver superior results.
This unified approach eliminates data silos and reduces training requirements since crews use familiar interfaces across all documentation tasks. Integration also enables sophisticated analytics that examine relationships between fire and EMS responses, resource utilization patterns, and community risk factors.
Breaking Down Documentation Silos
Traditional emergency service operations often maintain separate systems for fire incidents, EMS calls, training records, and administrative functions. This fragmented approach creates inefficiencies, increases error potential, and limits analytical capabilities that could improve service delivery.
Modern integrated systems address these challenges by providing unified platforms that maintain specialized functionality while ensuring data consistency and workflow integration. Crews benefit from single sign-on access and consistent user experiences, while administrators gain comprehensive operational visibility.

NEMSIS Compliance and National Data Standards
A critical factor in successful ePCR implementation involves ensuring compliance with NEMSIS standards that govern national EMS data collection and reporting. The 2024 NEMSIS Annual Report highlights ongoing challenges with data quality and standardization across jurisdictions.
Agencies implementing modern electronic patient care reporting systems benefit from built-in NEMSIS compliance features that automatically format data according to national standards. This compliance capability ensures seamless data submission to state and federal repositories while reducing administrative burden on EMS personnel.
Enhanced Data Quality Through Standardization
NEMSIS compliance extends beyond regulatory requirements to improve operational decision-making through standardized data collection. When agencies collect consistent, high-quality data, they can benchmark performance against national averages, identify improvement opportunities, and support evidence-based protocol development.
Research published in Taylor & Francis journals demonstrates that agencies using NEMSIS-compliant systems report higher data quality scores and more complete patient care documentation compared to those using non-standardized approaches.
Understanding This Composite Case Study Methodology
This analysis represents a composite case study methodology drawing from multiple data sources to present representative implementation outcomes for mid-sized EMS agencies. The approach combines:
Primary Research Sources:
- NEMSIS national database statistics representing over 60 million EMS activations
- Academic research on ePCR implementation from peer-reviewed medical journals
- NAEMT workforce engagement surveys covering industry trends and challenges
- NEMSIS data quality research on standardization benefits
Implementation Data:
- Documented performance improvements from agencies adopting electronic patient care reporting systems
- Industry benchmarks for documentation error rates and efficiency metrics
- Best practices identified through multiple successful deployments
Validation Methods:
- Cross-reference findings with published research on manual vs. electronic documentation
- Comparison with NEMSIS data quality initiatives and standardization efforts
- Alignment with established patterns in healthcare technology adoption
This methodology ensures findings reflect realistic expectations for agencies considering similar improvements while maintaining accuracy and avoiding overstated claims.
Why These Results Are Replicable Across Agency Types
The composite case study represents typical mid-sized agencies facing common documentation challenges, making these success patterns particularly relevant for other organizations considering similar improvements. Results align with broader industry trends toward electronic documentation and digital transformation in emergency services.
The 2024 NEMSIS dataset demonstrates widespread adoption of electronic patient care reporting across the United States, with over 14,756 agencies contributing standardized data. This growing adoption reflects recognition that modern EMS reporting software delivers tangible benefits for patient care, operational efficiency, and regulatory compliance.
Scalability Across Agency Types
Documentation challenges exist across agency types and sizes. Rural volunteer services struggle with limited administrative resources, urban departments manage high call volumes, and specialty transport services navigate complex billing requirements. Electronic patient care reporting systems address these varied needs through configurable solutions that adapt to specific operational requirements.
Technology Adoption Trends
Industry trends indicate that the majority of EMS agencies plan to upgrade their documentation systems within the next three years, driven by regulatory requirements, staff retention challenges, and operational efficiency demands reflected in NAEMT workforce surveys. This widespread interest in modernization creates opportunities for knowledge sharing and best practice development across the emergency services community.
What Does the Future Hold for EMS Documentation?
Electronic patient care reporting continues evolving with emerging technologies that promise even greater accuracy and efficiency improvements. Artificial intelligence integration enables predictive text completion, automated clinical decision support, and real-time quality monitoring that prevents errors before they occur.
Voice recognition technology allows hands-free documentation during transport, while mobile device integration ensures seamless data capture regardless of network connectivity. These technological advances build upon the foundation established by current electronic patient care reporting systems to create even more robust documentation solutions.
Forward-thinking agencies plan to expand their ePCR capabilities with integration to hospital electronic health records, enabling direct data transfer that eliminates handoff communication gaps. Predictive analytics features could identify patients at risk for repeat emergencies, supporting community paramedicine initiatives.
The trend toward enhanced operational efficiency through NERIS compliance demonstrates how modern platforms integrate multiple emergency response standards into unified solutions that benefit both fire and EMS operations.
Frequently Asked Questions
How long does it typically take to implement new EMS reporting software?
Implementation timelines vary based on agency size and complexity, but most organizations complete deployment within 3-6 months. This includes system configuration, staff training, data migration, and workflow optimization. Agencies benefit from phased rollouts that allow gradual adaptation while maintaining operational continuity.
What specific features should EMS agencies prioritize when selecting ePCR software?
Essential features include NEMSIS compliance, real-time validation tools, mobile device compatibility, integration capabilities with medical devices, customizable reporting templates, and robust data backup systems. Agencies should also evaluate vendor support quality, training resources, and system scalability for future growth.
How do electronic patient care reporting systems impact patient privacy and data security?
Modern systems incorporate advanced encryption, access controls, and audit trails that exceed traditional paper-based security measures. Cloud-based solutions provide redundant data backup, disaster recovery capabilities, and compliance with HIPAA requirements. Regular security updates and monitoring ensure ongoing protection against evolving threats.
Can smaller EMS agencies afford comprehensive electronic documentation systems?
Cloud-based subscription models make advanced EMS reporting software accessible for agencies of all sizes. These solutions eliminate infrastructure costs, provide automatic updates, and scale pricing based on call volume. Many agencies find that efficiency gains and improved billing accuracy offset system costs within the first year.
Transform Your EMS Documentation Today
This composite analysis demonstrates that implementing modern electronic patient care reporting systems delivers measurable improvements in accuracy, efficiency, and staff satisfaction. The documented 40% reduction in documentation errors represents just one example of the transformative potential available to agencies ready to modernize their operations.
For EMS agencies seeking to replicate these results while addressing their unique operational needs, comprehensive evaluation of available solutions is essential. Consider systems that integrate seamlessly with existing workflows while providing the scalability and functionality required for long-term success.
Understanding why integrated software solutions make a crucial difference in departmental operations can help agencies make informed decisions about their technology investments.
Ready to transform your agency’s documentation processes? Contact EPR Fireworks today to explore how their integrated EMS and fire department records management platform can streamline your operations, reduce errors, and improve patient care outcomes.

